Rising death rates, high levels of obesity, and gaps in care are pressing challenges for states
50%
increase in deaths from suicide, alcohol, and drug use since 2005
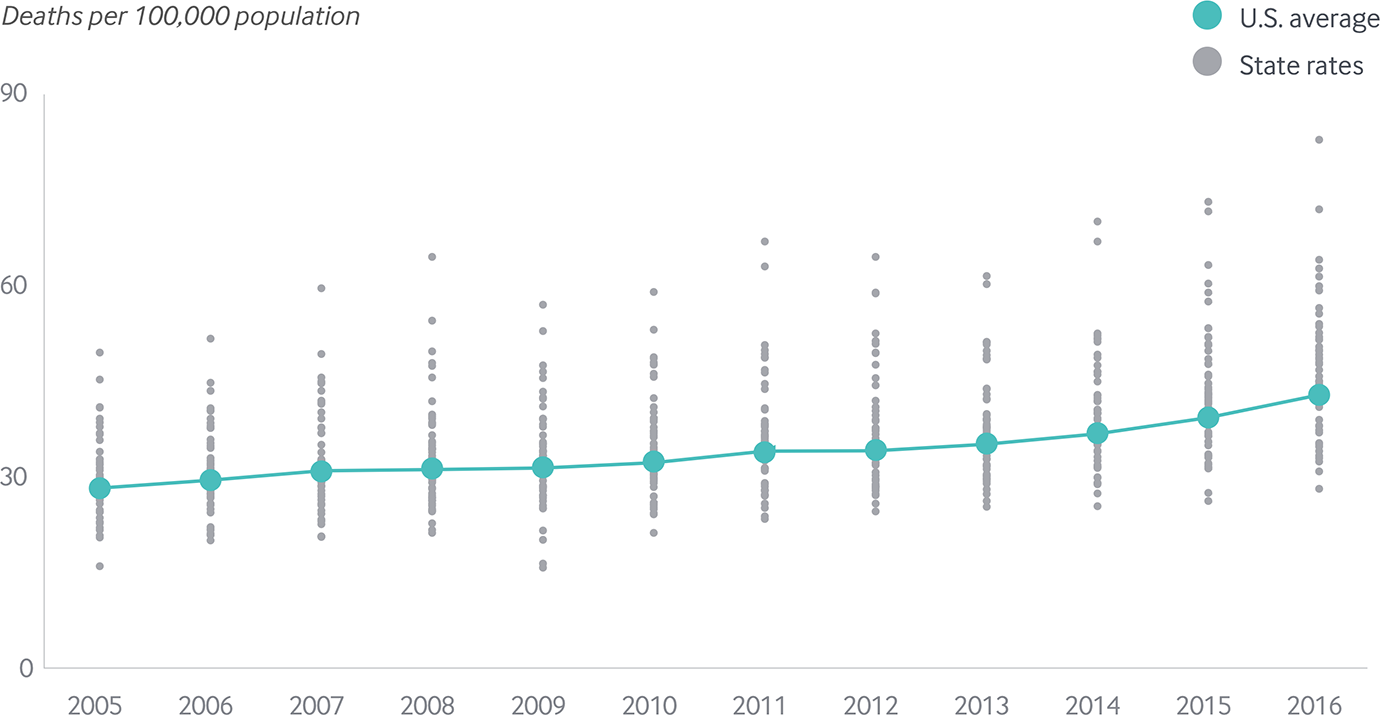
Deaths from suicide, alcohol, and drug use are at an all-time high
In 2016, average life expectancy at birth in the United States declined for a second year in a row, driven in large part by a spike in deaths from opioid and other substance abuse as well as suicide.1
The combined rate of deaths from suicide, alcohol, and drug use — sometimes referred to as “deaths of despair”2 — increased 50 percent from 2005 to 2016. Rates rose in all states, doubling or more in Delaware, New Hampshire, New York, Ohio, and West Virginia.
Deaths from suicide, alcohol, and drug overdose on the rise and differences between states widening
Share
Premature deaths are on the rise
After trending downward for most of the past decade, rates of premature death from preventable or treatable causes (a measure called “mortality amenable to health care”3) ticked upward nationally.
Two-thirds of states experienced an increase in 2014–15. In six states — Colorado, Maine, Nebraska, Oklahoma, Vermont, and Wyoming — the increase was greater than 5 percent. Compared to mortality rates in 2012–13, the higher rates in 2014–15 represented a sobering number of additional premature deaths: 351 in Colorado, 643 in Oklahoma, and 988 in Texas, for example.
Premature death rates from treatable medical conditions rose slightly following decade-long decline
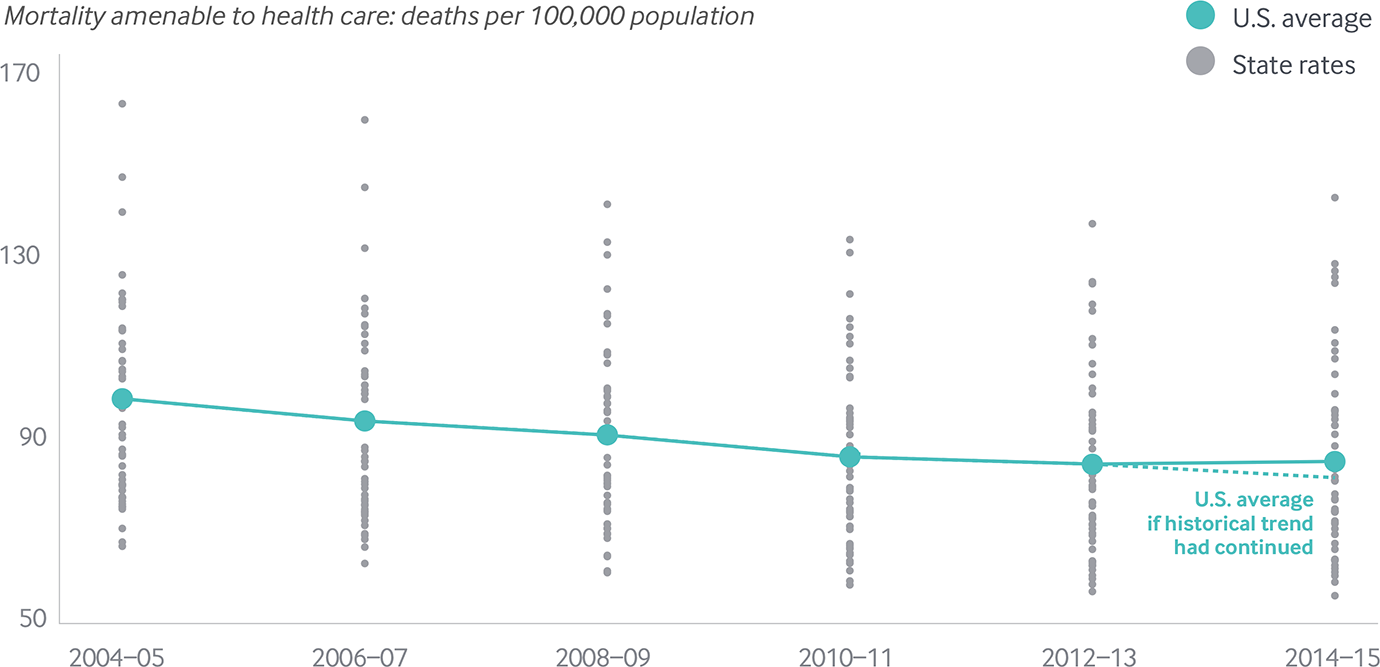
Notes: Y-axis starts at 50 deaths per 100,000. Dashed line represents the expected premature death rate if the historical trend from 2004–05 to 2012–13 had continued in 2014–15. Premature deaths reported here do not include deaths from suicide, alcohol, or drug use; see Appendix H for a complete list of health care–amenable deaths.
Data: 2004–2015 National Vital Statistics System (NVSS) Mortality All-County Micro Data Files.
Share
Obesity represents a rising public health threat
In Mississippi and West Virginia, the proportion of obese adults reached 39 percent in 2016. Even in states with the lowest rates, a quarter of adults are obese.
Gaps in mental health care are pervasive
Up to one-quarter of adults with a mental illness reported a need for care that wasn’t met during the 2013–15 period.
Meanwhile, up to one-third of children needing mental health treatment in 2016 did not receive it, according to their parents. Across states, 41 percent to 66 percent of adults with symptoms of a mental illness (some of whom may not have been diagnosed) received no treatment in 2013–15.
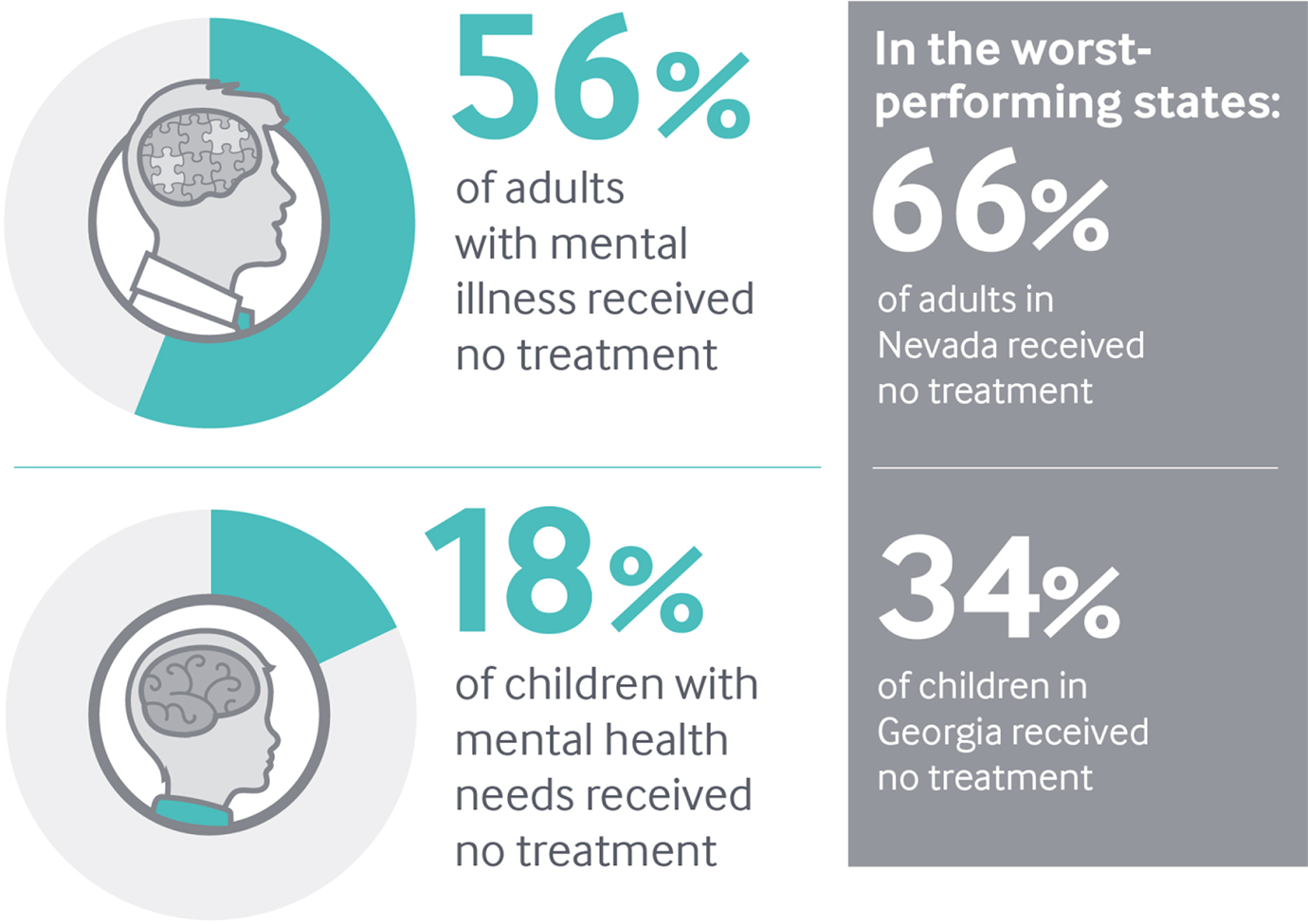
Data: 2013–15 National Survey of Drug Use and Health, as reported in The State of Mental Health Care in America, 2017; 2016 National Survey of Children’s Health, as reported by the Child and Adolescent Health Measurement Initiative.
Share
What Can Be Done?
Reversing these trends and closing gaps in care will likely require cooperation across sectors as well as greater integration of medical, behavioral, public health, and social services.4
What Are States Doing?
Some states and Medicaid managed care organizations are realizing the importance of investing in, and fostering linkages to, social services in the community that can address the “social determinants of health,” such as stable housing and access to nutritious food.5
Medicaid programs are starting to integrate behavioral and physical health care, for example, by establishing “health homes” where teams of health professionals deliver coordinated care for patients with chronic illnesses and provide screenings, referrals to substance abuse treatment, and other services.6