States made progress in areas that were the target of efforts to improve
20%
reduction since 2011 in the share of adults who smoke
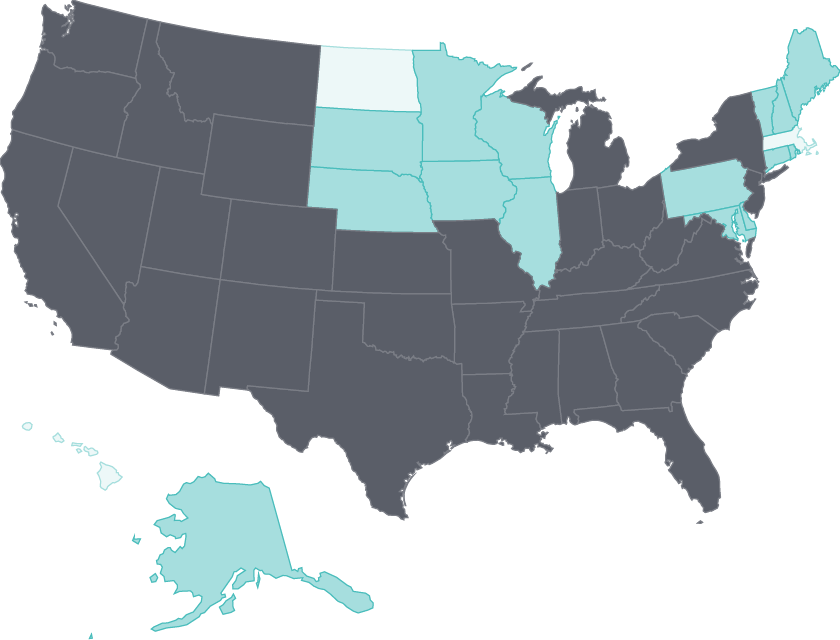
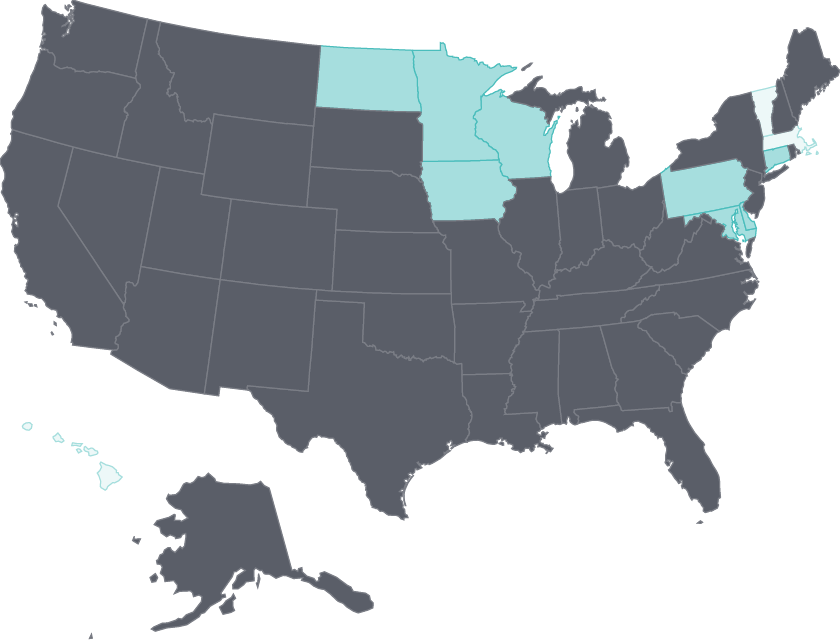
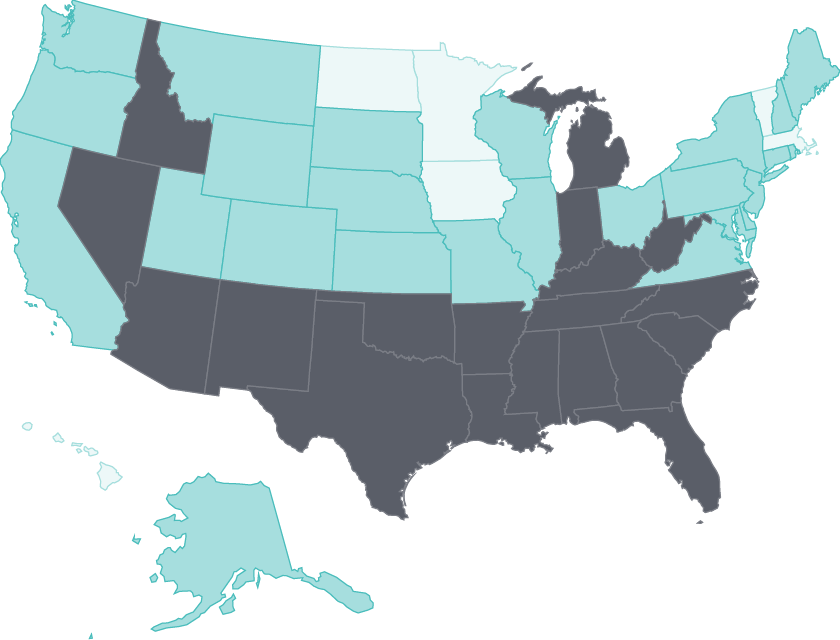
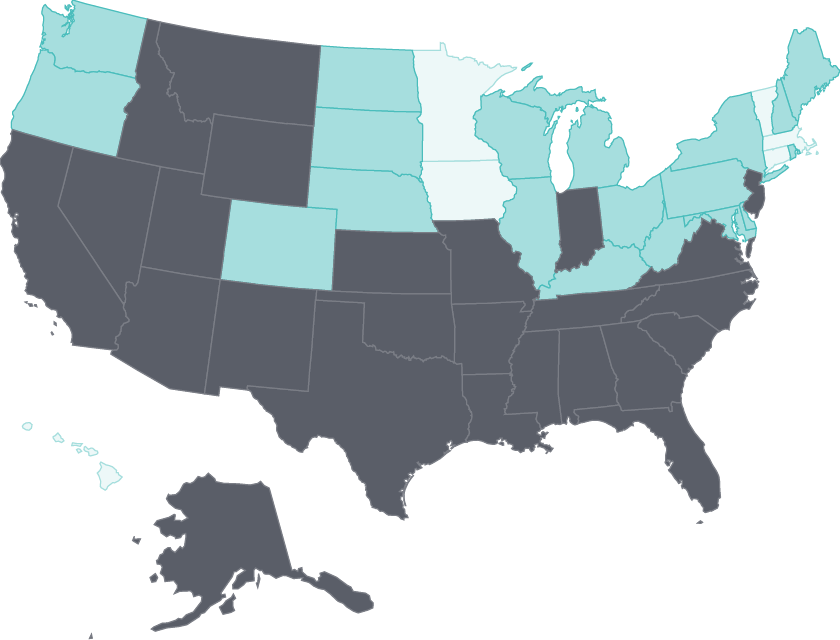
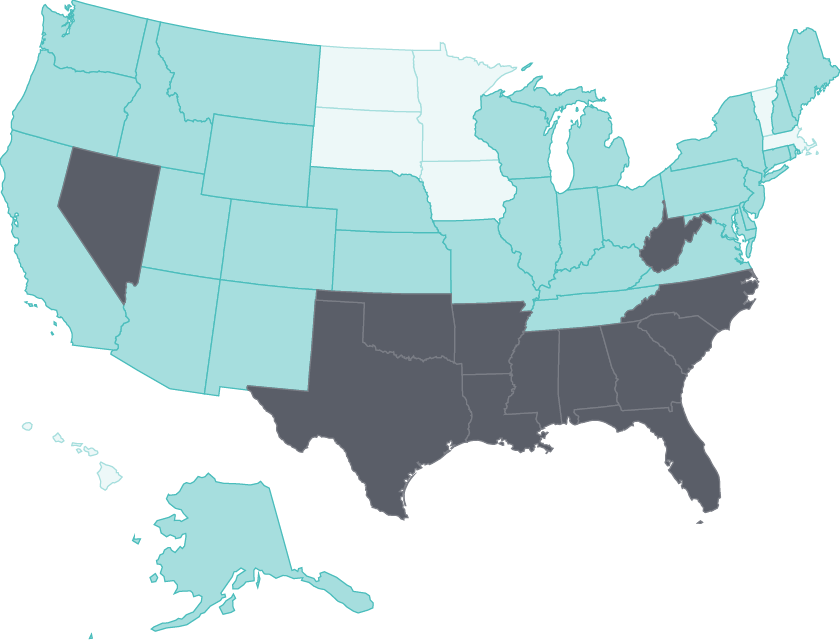
There have been widespread gains in health care access
During the first three years of the Affordable Care Act’s major insurance coverage expansions, the adult uninsured rate declined by at least five percentage points in 47 states.
And in nearly three-quarters of states, substantially fewer adults skipped needed care because of costs. States that expanded their Medicaid programs have made the largest gains.26
Cost barriers to receiving care fell as uninsured rates fell following ACA coverage expansions
- Select a year to see changes over time.
Uninsured adults
2011 Adults who went without care because of costs
2011
- Less than 10%
- 10%-14%
- 15% or more
Share
Nursing home care has improved, and home health patients have gained physical mobility
The percentage of home health patients who got better at walking or moving around — a key measure of quality of care — rose substantially in every state. In nursing homes, the potentially harmful use of antipsychotic drugs as “chemical restraints” has fallen in nearly all states. This change likely reflects the goals of the National Partnership to Improve Dementia Care in Nursing Homes, which supports state-based coalitions in efforts to reduce inappropriate antipsychotic drug use and improve care for residents with dementia.27
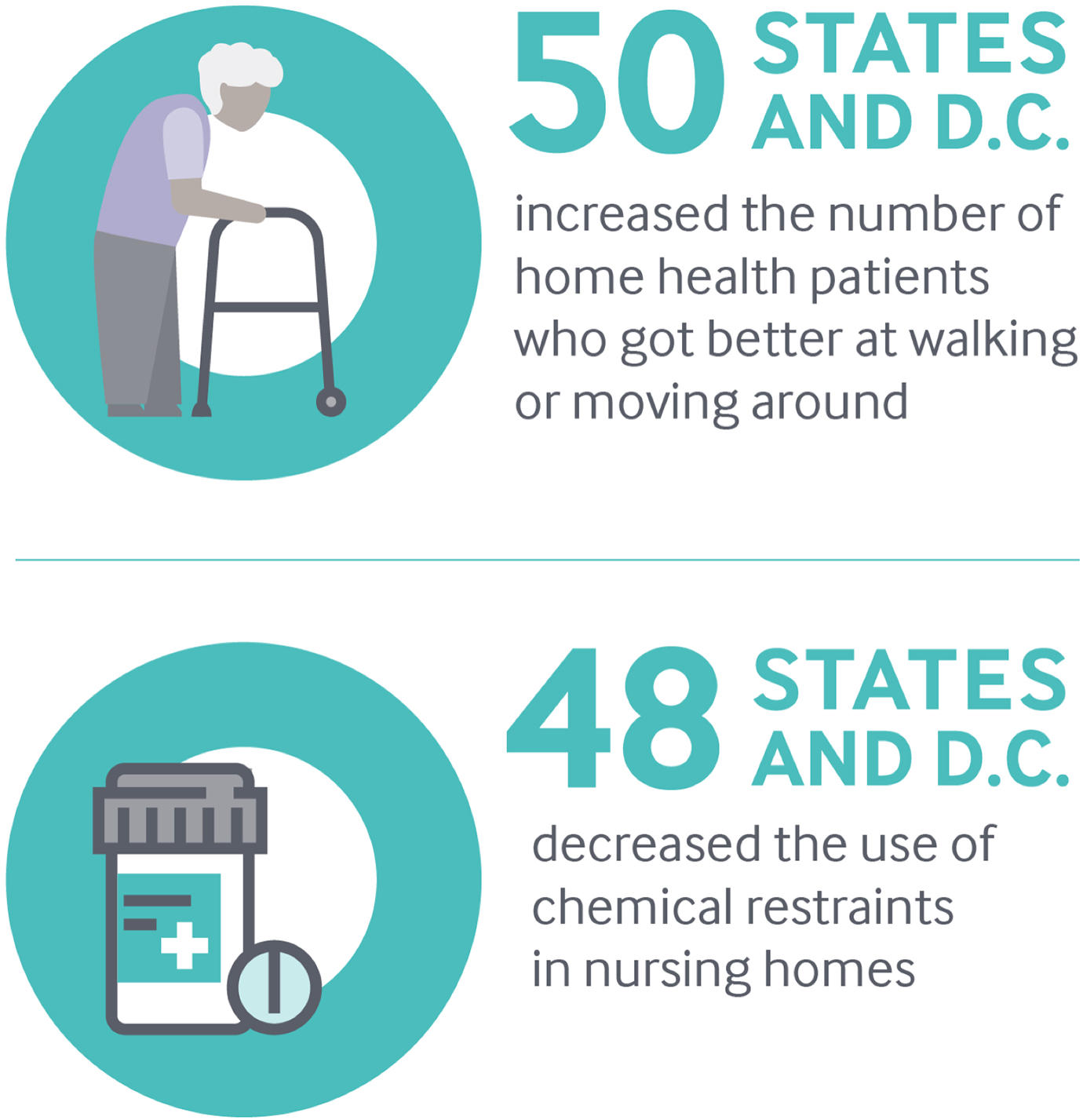
Notes: Chemical restraints means use of antipsychotic medication.
Data: OASIS (via CMS Home Health Compare); MDS (via CMS Nursing Home Compare).
Share
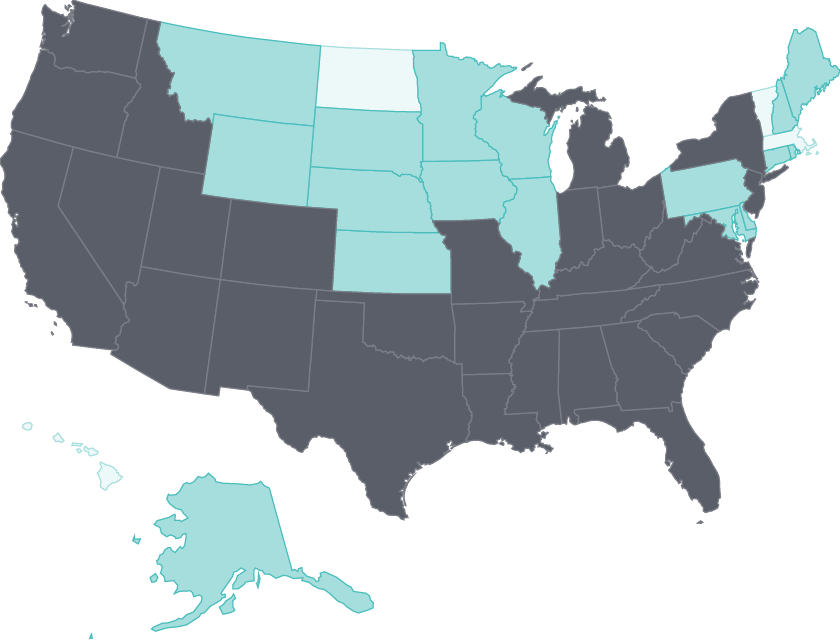
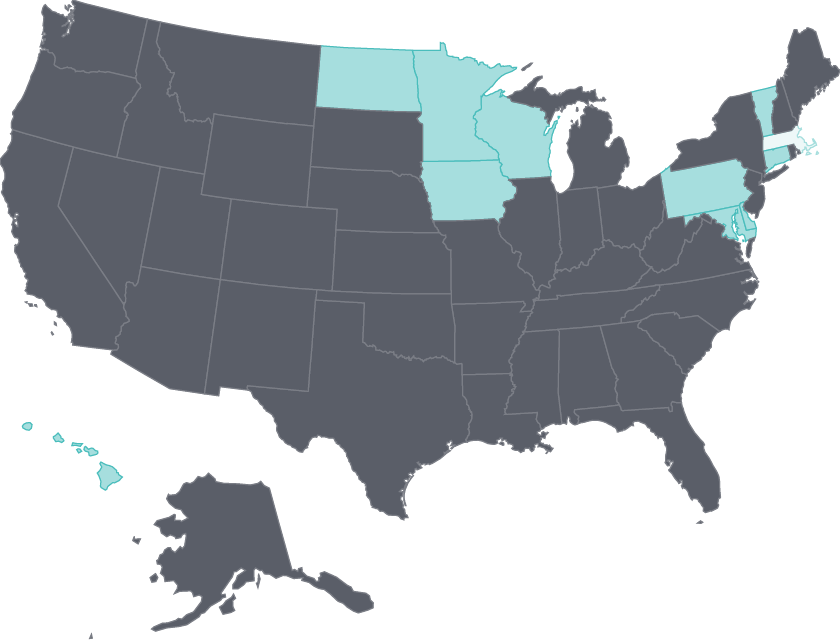
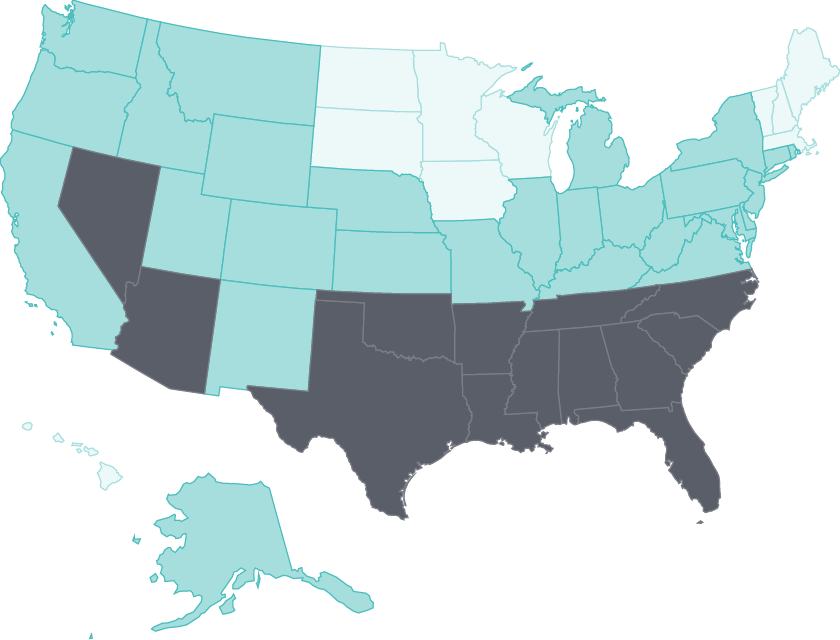
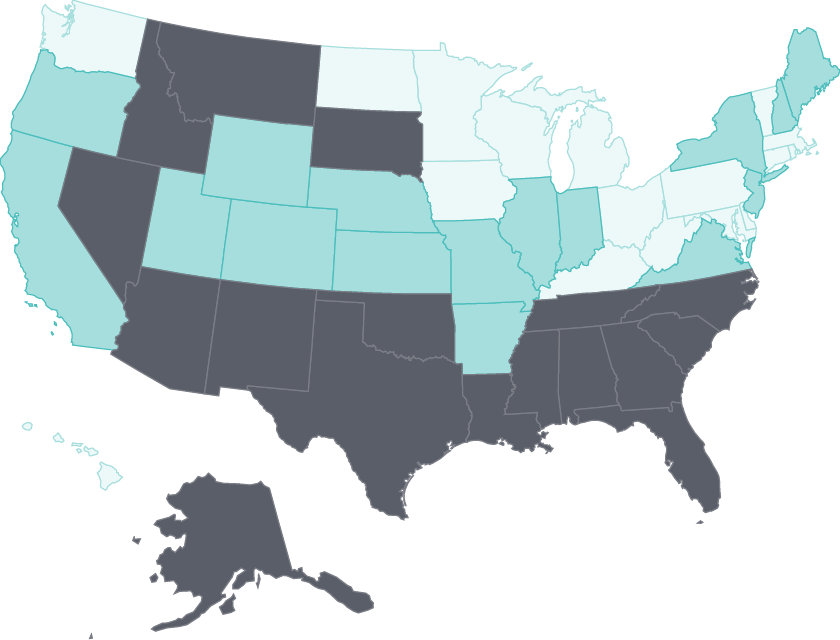
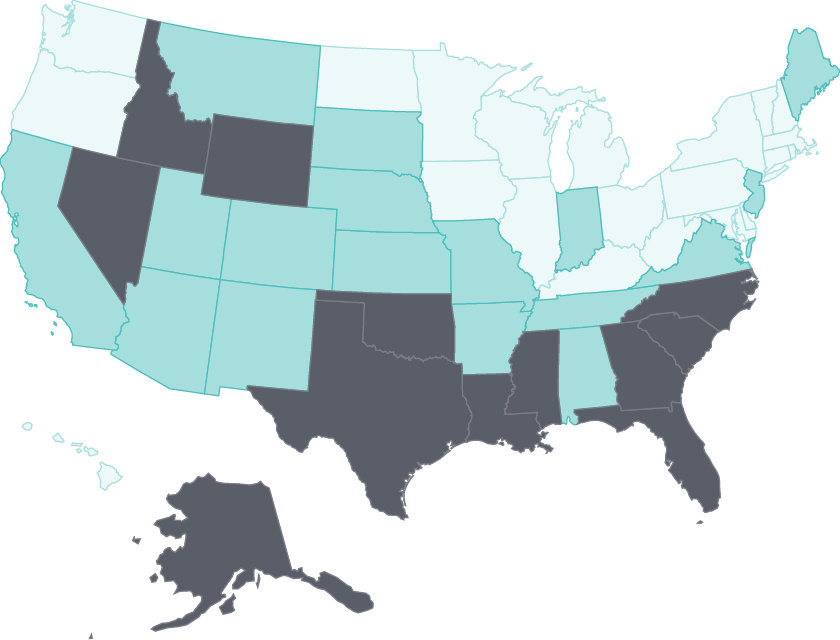
Tobacco use continues to wane
Adult smoking rates fell by at least three percentage points in all but four states between 2011 and 2016.
States with some of the highest rates, such as Nevada and Oklahoma, saw the largest declines.28 States like California with long-standing comprehensive tobacco control policies have seen substantial reductions in health care spending because of lower smoking rates.29 Limiting tobacco use continues to represent a major opportunity for states to improve public health.30
Tobacco use continues to decline: Nevada and Oklahoma had among the largest reductions in adult smoking between 2011 and 2016
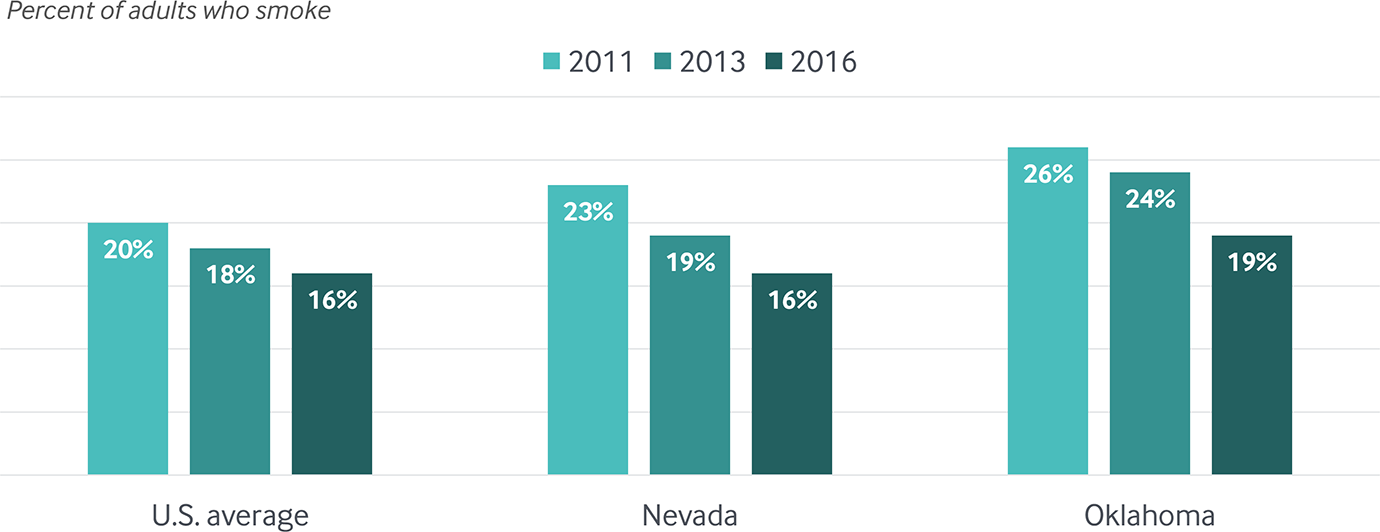
Data: 2011, 2013, and 2016 Behavioral Risk Factor Surveillance System (BRFSS).
Share
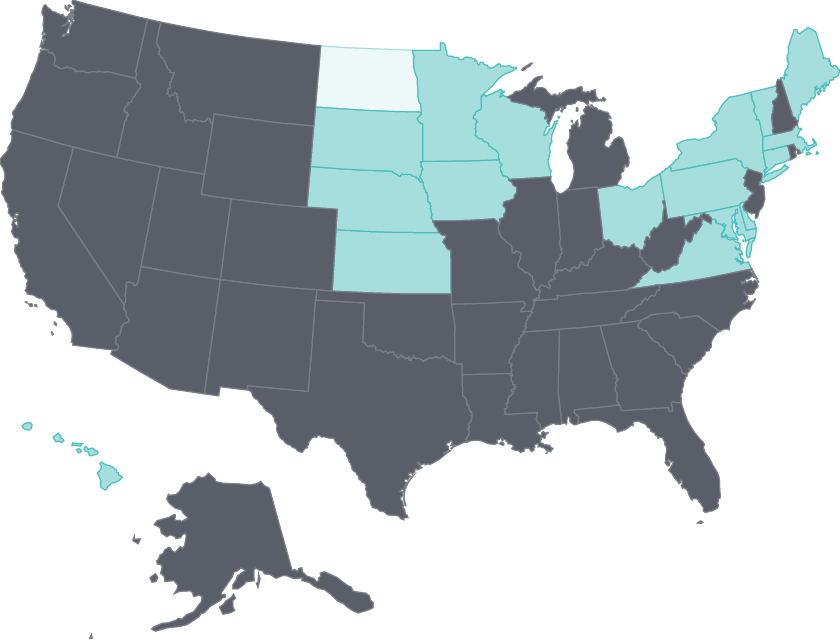
Avoidable hospital use has declined
Hospital readmission rates for elderly Medicare beneficiaries continued to fall in nearly half the states (particularly those with the highest rates) during the 2012–15 period.
This reduction was the goal of federal financial penalties, as well as initiatives that brought hospitals and postacute care providers together to improve patients’ transitions in care.31 There was also a continuing reduction in potentially preventable hospital admissions in several states, possibly because of better ambulatory care management.
What Is Being Done?
States’ gains likely reflect the influence of government policies, regulatory actions, and collaborative improvement efforts, all of which may be reinforced by the public reporting of performance data by the federal government, states, and other groups.
With federal assistance, many states also are working with health plans, care providers, and other stakeholders to promote quality measurement and improvement in Medicaid and to spread payment and delivery system transformation more broadly.32
At the same time, recognition that performance incentives can sometimes be gamed, or can unfairly penalize providers treating a large share of vulnerable or high-need patients, is prompting discussions of how to improve these incentives.33