Many states are not getting good value for their health care dollars
29%
of adults with job-based insurance received unneeded lower back imaging at diagnosis
Quality of care is not in line with the level of state health spending
Health care spending in the United States is much greater than in other wealthy countries, but U.S. health outcomes are not better.13
Our analysis finds that for every state, health spending exceeds median per capita spending in each of 10 other high-income countries.14 In general, research shows that higher spending in the U.S. is attributable to higher prices.15
Here are just a few examples of gaps in quality across the U.S.:
- Among working-age adults with employer-sponsored insurance, nearly one in three (29%) who were newly diagnosed with lower back pain in 2015 received potentially inappropriate medical imaging. That means the scans these patients received are not associated with improved outcomes when there is no underlying condition; some tests would expose them to unnecessary radiation.16
- One in three adults were not up to date on recommended cancer screenings in 2016. Even in the best-performing state, the shortfall was 24 percent. As many as 40 percent of adults in Idaho, New Mexico, Oklahoma, and Wyoming did not get these screenings.
- Even when they have insurance coverage, Americans visit the emergency department (ED) for nonemergency care at high rates. Similarly high rates among Medicare- and employer-insured adults suggest there may be factors other than coverage or age, such as inadequate access to primary care, driving the behavior.
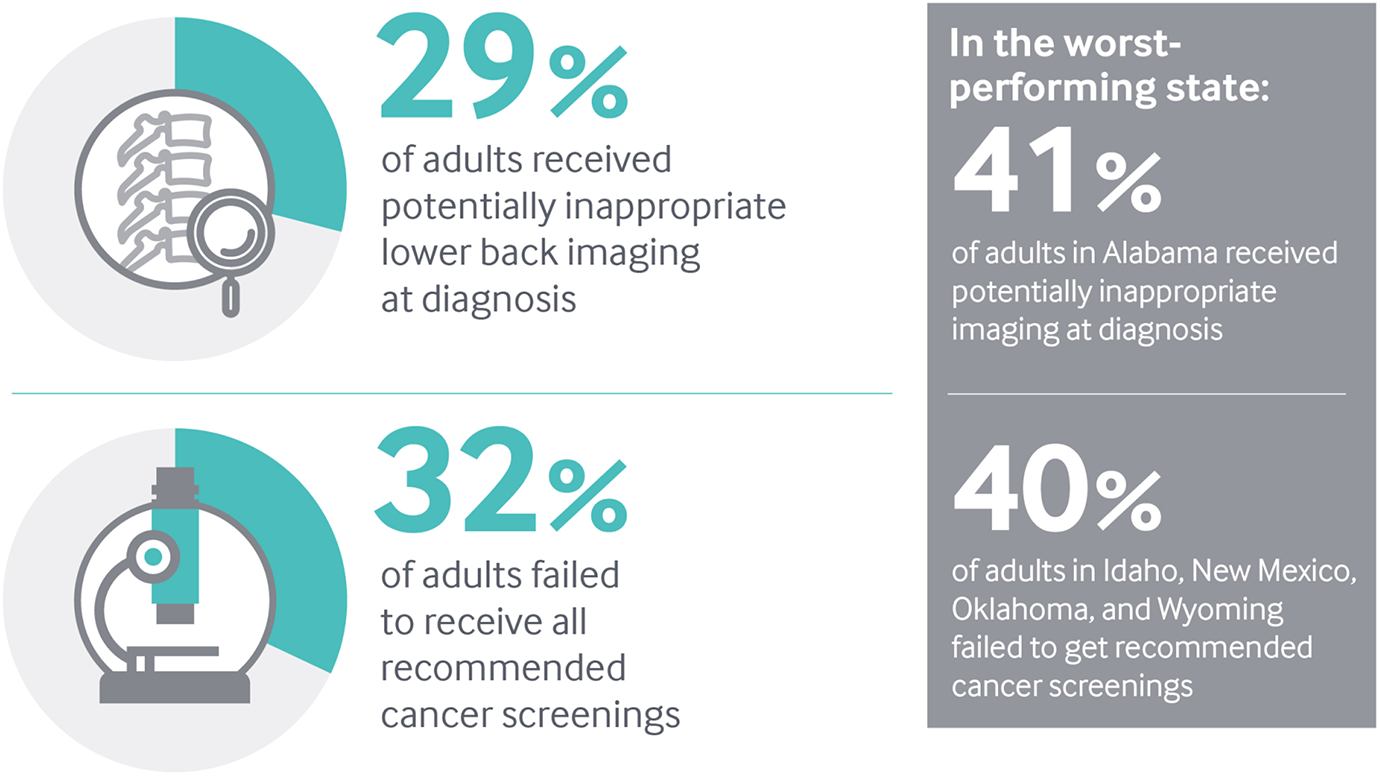
Note: Lower back pain imaging is measured among newly diagnosed working-age patients ages 18–50 with employer-sponsored insurance.
Data: Lower back imaging, 2015 Truven MarketScan Database, analysis by M. Chernew, Harvard University; Cancer screenings, 2016 Behavioral Risk Factor Surveillance System (BRFSS).
Share
Mixed findings on health care spending
The average amount Medicare spends on care for each beneficiary has leveled off in recent years across all states.
Spending per enrollee in employer-sponsored insurance plans was nearly flat nationally from 2013 to 2015. However, 18 states saw increases of at least $300 per enrollee during this time, or 5 percent on average — more than twice the rate of general inflation.17 These data do not include prescription drug costs, which have been rising rapidly in recent years. Both across states and within individual states, there is often no consistent relationship between health care spending by Medicare and by employer-sponsored insurance.18
What Can Be Done?
Efforts to control health care costs must be tailored to reflect the unique characteristics of each market.19
Greater pricing transparency, coupled with value-based benefit design and payment approaches, could encourage better-informed choices and movement toward higher-value health services and providers.20 Evidence from states and from countries around the world show that health systems with a strong primary care orientation generally achieve better health outcomes at lower cost.21 Making primary care more accessible and patient-centered also can help reduce use of the ED for conditions that could be treated in primary care settings.22
What Are States Doing?
Several states participate in initiatives involving both public and private insurers to foster the transformation of primary care practices into patient-centered medical homes, which can improve patient care and reduce costs.23
State and federal partnerships to integrate care for Medicare and Medicaid beneficiaries aim to reduce hospitalizations and ED use among patients with complex care needs while improving their quality of life.24 In Rhode Island, health plans are required to measure and increase the proportion of health care spending devoted to primary care, without increasing medical costs or premiums.25