A Closer Look:
New Hampshire and Maine:
Two States Where Medicaid Expansion Is in Flux
Before the Affordable Care Act expanded coverage, New Hampshire greatly lagged Maine in terms of access to health care for low-income adults. But in August 2014, New Hampshire expanded its Medicaid program and has since caught up to its New England neighbor, matching Maine on its uninsured rate among low-income adults and nearly closing the gap on several other key Scorecard measures of health care access. Maine has not only failed to take advantage of its early lead, it has lost ground on some measures.
In November 2017, Maine residents voted to expand Medicaid under a citizen-initiated ballot referendum. The expansion is estimated to extend Medicaid coverage to 70,000 to 80,000 Mainers45 with incomes up to 138 percent of the federal poverty level ($16,753 for a single person in 2018), although implementation has been stalled because of funding conditions set by the governor. New Hampshire is facing the expiration of its Medicaid expansion in December 2018, and it’s not clear whether the state legislature will reauthorize it. The result could be a loss of coverage for an estimated 50,000 Granite State adults.46
The Scorecard offers an inkling of what New Hampshire could lose by dropping Medicaid expansion and what Maine might gain by adding it.
Adult uninsured rates drop more in New Hampshire than in Maine
Although the low-income adult uninsured rate fell to 20 percent in both states in 2016, in New Hampshire, this represented a 14 percentage point drop from its 2013 rate. Maine saw a 6 percentage point decline in the same time period.
Income-related disparities in health care access differ across states
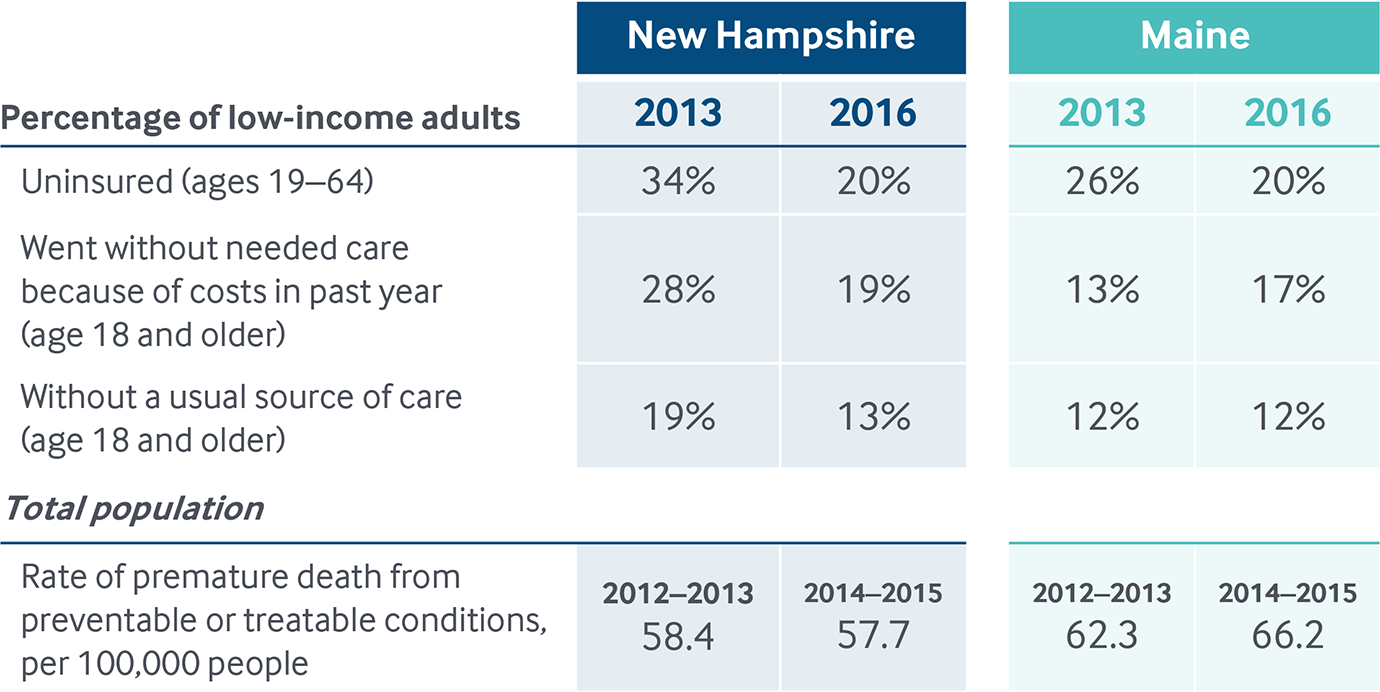
Notes: Low-income is < 200% of the federal poverty level. The difference between the 2013 and 2016 rates in New Hampshire on all three access indicators among low-income adults meet the Scorecard’s threshold for improvement for these indicators, as does the does the difference in Maine in uninsured rates. The increase in low-income adults who went without care because of costs in Maine meets the Scorecard’s threshold for worsening on this measure. See Scorecard Methods and Appendix H for more detail.
Data: Uninsured, U.S. Census Bureau, 2013 and 2016 One-Year American Community Surveys. Public Use Micro Sample (ACS PUMS); Cost barriers, 2013 and 2016 Behavioral Risk Factor Surveillance System (BRFSS); Premature death, 2012–2015 National Vital Statistics System (NVSS) Mortality All-County Micro Data Files.
Number of people skipping care because of costs drops in New Hampshire, increases in Maine
New Hampshire saw a 9 percentage point reduction in the share of low-income adults age 18 and older who reported not going to the doctor when needed because costs were too high. In Maine, the share of adults with low incomes who said they skipped needed care because they couldn’t afford it increased 4 percentage points between 2013 and 2016.
Share of low-income adults without a usual source of care drops in New Hampshire, stays the same in Maine
New Hampshire also nearly caught up with Maine on another key measure of health care access: having a regular doctor or health care provider. The share of low-income adults age 18 and older who did not have a usual source of care decreased 6 percentage points in New Hampshire between 2013 and 2016; the rate remained unchanged in Maine.
Premature death rates rise in Maine, decrease in New Hampshire
In Maine, the rate of premature death from preventable or treatable causes — a measure called “mortality amenable to health care” in the Scorecard — increased from 62.3 to 66.2 per 100,000 people between 2012–2013 and 2014–2015. This represented a 6.3 percent increase — one of the highest in the nation. Only three states saw larger relative increases. New Hampshire, on the other hand, was one of only 14 states that saw a decline in this rate, with a drop from 58.4 to 57.7 per 100,000 people, about a 1.1 percent decline.