Digital health technologies encompass a wide variety of tools, ranging from wearable sensors and portable diagnostic equipment to data-driven software platforms, telemedicine tools, and mobile health care apps. Together, they have the potential to help the U.S. health care system achieve five important goals:
- helping patients become more engaged in their own care
- closing communication gaps
- identifying patients' needs and tailoring services to meet them
- enabling consumers to get care in convenient, cost-effective ways
- improving decision-making by consumers and providers.
Consider the case of Harold Goldmann, diagnosed with heart failure at age 88. After a home health nurse counseled him on the dangers of salt and when to call 911, Goldmann—already feeling isolated and scared—became convinced that any misstep on his part could result in death. Connections to his care team, enabled by remote monitoring devices, became his lifeline.
Goldmann learned to use a pulse oximeter and blood pressure cuff to monitor his condition and transmit the findings through a phone line. He also used videoconferencing to build a strong bond with a nurse, who helped him understand when his measurements were within normal limits.
Remote monitoring devices such as these can help patients understand their conditions and gain the confidence to manage them. At the same time, they can signal to providers when a problem emerges and help prevent serious complications. They also allow providers to monitor how well patients are doing between office visits, and reveal living conditions that affect health outcomes.
Closing Communication Gaps
Some approaches use technology that's already in our hands, like smartphones and tablets, to improve communication between and among patients and providers.
Researchers at the Center for Connected Health found that giving teenage asthmatics a shared Facebook page, or sending people with diabetes customized text messages encouraging healthy behaviors, can lead to better health. Meanwhile, the University of California, San Francisco’s Center for Digital Health Innovation has created a CareWeb app that unites information streams from multiple sources into a single, secure, discussion thread—much the way Twitter and Facebook do—so that patients, their caregivers, and teams of providers can easily share information and take action quickly.
Detecting Health Declines
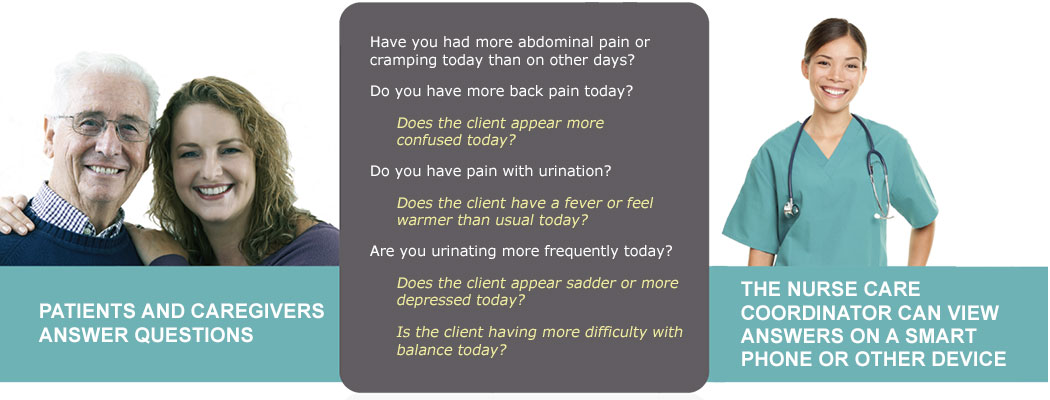
Care at Hand—a cloud-based platform used on a tablet or phone—collects observations from home care workers and other professionals about their patients' health and living conditions. Through a series of algorithm-driven prompts, the tool helps caregivers detect symptoms that may indicate a deteriorating condition, safety risk, or unmet need. Responses can trigger an alert to a supervising nurse care manager or lead to other types of support.
Tailoring Services
Data-driven technology can help clinicians deliver smarter care. For example, clinical researchers are mining data from electronic medical records, medical journals, and other sources to find out which interventions really work and when they should be deployed. At Stanford University's Clinical Excellence Research Center, social scientists, engineers, and clinicians used this approach to redesign care for patients with chronic kidney disease (CKD).
A review of CKD treatment approaches suggests that outcomes can be improved and costs reduced if new care delivery methods are implemented shortly after diagnosis and at the time patients begin to experience severely reduced kidney function. Coupled with efforts to coordinate care through a nurse caregiver, group visits with specialists via videoconference, and shared decision-making around dialysis options, such carefully timed interventions have been found to slow the disease's progression, reduce emergency department visits, and lead to greater use of safer and less costly end-stage treatment methods (such as home-based dialysis).
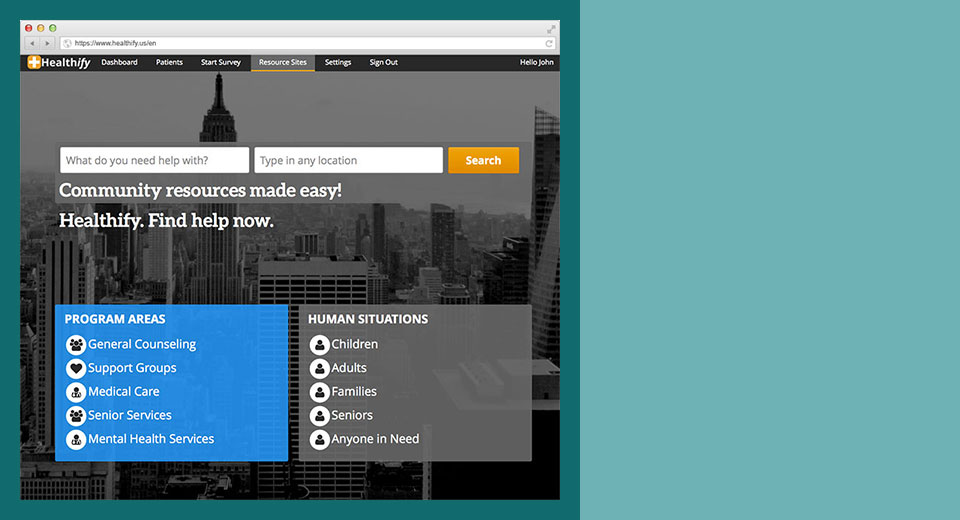
Data-driven tools are also being put to work to help providers take note of and address patients' nonmedical needs—for safe housing, sufficient food, child care, behavioral health care, or other factors that have an outsized impact on health.
Healthify, a startup founded by Johns Hopkins University graduates and students, gives providers a screening tool to identify patients’ social needs, then uses an algorithm to find community-based organizations that may be able to help.
Convenient, Cost-Effective Care Models
Digital tools can also pave the way for more convenient, cost-effective care delivery models. Increasingly, consumers are able to consult with a physician or nurse practitioner via video or Web-based platforms to diagnose conditions that often require little more than a medical history to assess, such as pink eye, insect bites, and bladder infections. Such virtual consults are also being used in traditional health care settings to facilitate care for patients with complex conditions who need both primary care physicians and specialists present.
The Big White Wall, a Web-based platform developed in the United Kingdom and used by the National Health Service (NHS), allows consumers to access educational material on behavioral health issues, obtain peer support, and interact with providers who offer live therapy via video, text, and audio—all while having the privacy and convenience of being in their own homes. The model, which has produced $540 in savings per NHS member per year, could be used in rural U.S. communities, where shortages of mental health professionals and privacy concerns sometimes deter people from seeking help.
Improving Decision-MakingTechnology can also help people make sense of their conditions, sort through their treatment options, and make wise decisions about their care. Decision aids, including interactive tools and Web-based educational resources, have been shown to both increase patients' knowledge about their care and improve their satisfaction. Some tools provide comparative information about the quality and costs of care. The
Change Healthcare tool alerts people by text or email if they have an opportunity to save money on routine care or prescription drugs. For example, a message might say, "You can save $250 a year on your health care costs," and then provide instructions for making the switch to a lower-cost provider.
Targeting the Greatest NeedsTo be sure, not all digital health technologies will add value or promote better health. Many will fail to take root because their developers have focused on technological solutions, without fully understanding the problems they seek to address or the complexity of clinical workflows and regulatory requirements.
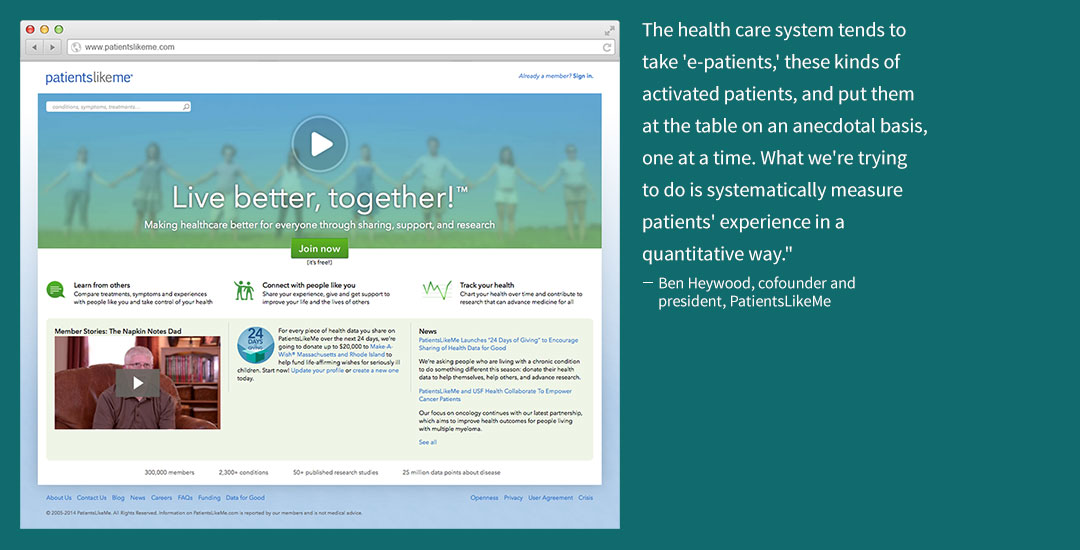
To ensure that new digital health tools solve real needs, it’s important to listen to what consumers—and patient advocates like Morgan Gleason—say matters to them. The platform
PatientsLikeMe provides a wealth of information about patients' experiences that is fueling research into better disease management and more effective treatments.
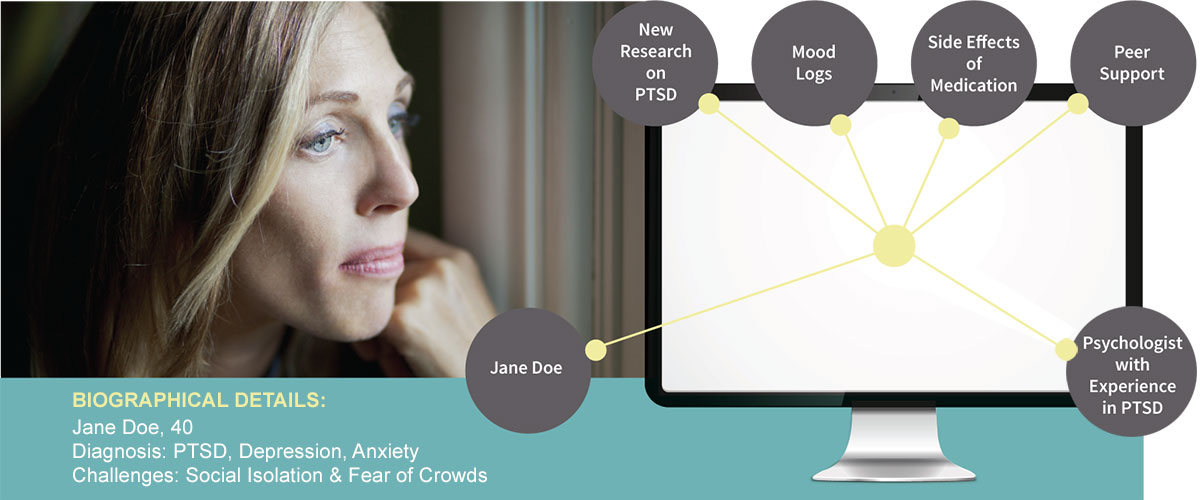
It's also important to focus on populations with significant needs, including the growing number of people with chronic or complex conditions. These individuals are perhaps the most likely to benefit from streamlined communication with their providers, better care coordination, help with managing medical information, and encouragement to engage in self-care.
Clearly, no one tool will slay all of health care's dragons. But new care delivery models that leverage the best of what technology can do—enabling connections, making sense of data, and instilling logic and consistency in complex systems—have the potential to make care more effective, more convenient, and of higher value to patients.